India’s Growing Cancer Burden:
- In 2022, India saw an estimated 1.46 million new cancer cases, with a crude incidence rate of 100.4 per 100,000 people. This means roughly 1 in 9 people in India are expected to develop cancer during their lifetime. The most common cancers in India are lung cancer in men and breast cancer in women.
- High proportion of cases continue to be detected at late stages for major cancer types in India.
- High burden of cancer incidence in India is resulting in a high economic burden on account of productivity losses and premature mortality.
The issue of high disease burden is compounded with late-stage detection caused mainly due to lack of awareness and low penetration of screening programs. India has a poor cancer detection rate of 29%, with only, 15% and 33% of breast lung and cervical cancers being diagnosed in stages 1 and 2, respectively, which is significantly lesser than that in China, the UK and the US.
While at one hand incidence is rising, deaths due to cancer has remained among the top 5 causes of deaths in India over the last decade. Estimates indicate that the total deaths due to cancer have been ~8 to 9 lakh in 2020, causing the mortality to incidence ratio for different cancer types in India being among the poorest compared to global counterparts.
Based on reported cancer incidence and mortality across age groups and years of potential productive life lost (YPPLL) due to the same, estimates indicate that the economic burden in terms of GDP losses is in the range of US$11B. (0.4% of national GDP) in 2020.
The same is projected to increase to US$36B to US$40B by 2030, driven by a projected increase in mortality, improvement in life expectancy and increase in GDP per capita.
Which Types Are Most Prevalent and Why?
In India, the incidence of cancer is rising alarmingly, with certain types becoming more prevalent due to a complex interplay of genetic, lifestyle, dietary, environmental, and healthcare factors.
Experts warn that even young Indians are increasingly being affected by cancers that traditionally impacted older populations. Lack of awareness, delayed diagnosis, and societal stigma continue to worsen outcomes. Here’s a detailed look at some of the most common cancers in India today:
Table of Contents
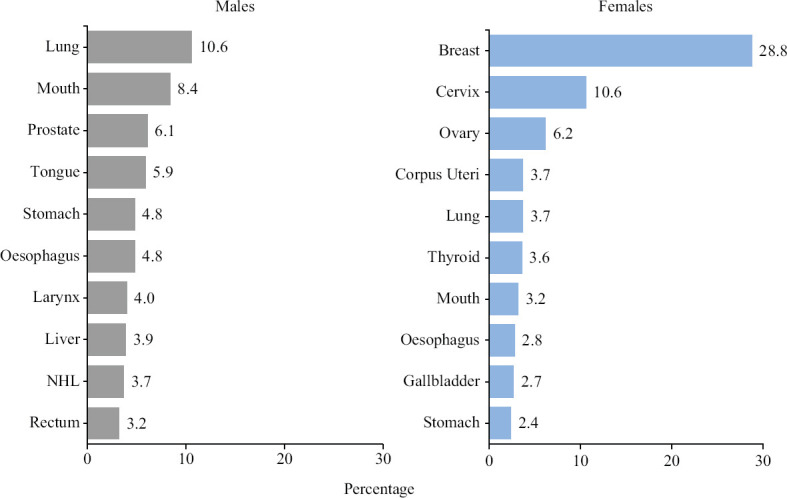
The National Cancer Registry Programme Report 2020, reported the cancer incidence from 28 Population-Based Cancer Registries (PBCRs) for the years 2012-2016. This was used as the basis to calculate cancer estimates in India.Fig. 1 presents the estimated top five leading sites of cancer; among males these were lung (10.6%), mouth (8.4%), prostate (6.1%), tongue (5.9%) and stomach (4.8%). The estimated top five leading sites of cancer among females included breast (28.8%), cervix (10.6%), ovary (6.2%), corpus uteri (3.7%) and lung (3.7%). Liver cancer (3.9%) was among the leading ten cancers in males and not in females, whereas thyroid (3.6%) and gallbladder (2.7%) cancers were in top ten among females but not in males.
- Breast Cancer: A Growing Concern Among Indian Women
- Oral Cancer: India’s Growing Crisis
- Lung Cancer: The Silent Killer
- Cervical Cancer: Preventable Yet Prevalent
Breast Cancer: A Growing Concern Among Indian Women
Breast cancer has emerged as one of the most significant health concerns among Indian women across all age groups. It accounts for a large percentage of all female cancers. Though less common, men can also develop breast cancer.
Doctors point to factors such as late marriages, fewer childbirths, absence of breastfeeding, and lifestyle changes contributing to the rise in breast cancer cases. Mammography remains one of the most effective diagnostic tools, capable of detecting breast cancer even before any noticeable lump forms.
How do healthcare providers diagnose Breast cancer?
Early detection remains the primary defense in preventing advanced breast cancer. Screening modalities include the following:
- Mammography
- Ultrasonography
- Magnetic resonance imaging (MRI) with and without contrast
- PET CT to know its spread
Ultrasonography and MRI are more sensitive than mammography for invasive cancer in nonfatty breasts. Combined mammography, clinical examination, and MRI are more sensitive than any other individual test or combination of tests.
Oral Cancer: India’s Growing Crisis
India is increasingly being referred to as the oral cancer capital of the world, primarily due to the widespread use of tobacco and alcohol. Smokeless tobacco products such as gutka and paan masala account for nearly 90% of oral cancer cases.
Apart from tobacco use, poor oral hygiene and unhealthy dietary habits also contribute to the problem. Health experts emphasize the urgent need for robust tobacco control measures, strict regulation on tobacco sales, and widespread public education to curb the rising cases.
How do healthcare providers diagnose oral cancer?
Your dentist may spot potential oral cancer during one of your regular checkups. They may follow up with preliminary tests or refer you to an oral and maxillofacial surgeon, or head and neck surgeon. These specialists are also called ear, nose and throat (ENT) specialists.
Oral cancer tests include:
- Physical examination: Your healthcare provider will look at the entire inside of your mouth and might feel around your mouth. They’ll also examine your head, face and neck for potential signs of pre-cancer or cancer.
- Brush biopsy also called scrape biopsy or exfoliative cytology: Healthcare providers use a small brush or spatula to gently scrape the area in question to obtain cells examined for cancer.
- Incisional biopsy: Your healthcare provider will remove small pieces of tissue to get cells to be examined for cancer.
- Indirect laryngoscopy and pharyngoscopy: Your healthcare provider uses a small mirror on a long thin handle to look at your throat, the base of your tongue and part of your larynx (voice box).
- Direct (flexible) pharyngoscopy and laryngoscopy: They may use an endoscope to look at areas of your throat and mouth that can’t be seen with mirrors. An endoscope is a thin, flexible tube with an attached light and viewing lens.
Lung Cancer: The Silent Killer
Lung cancer remains a leading cause of cancer-related deaths in India. The growing number of cases is largely attributed to tobacco use and environmental pollution.
How do healthcare providers diagnose lung cancer?
If a person has lung cancer symptoms or if screening shows something unusual, a healthcare professional may recommendTrusted Source the following diagnostic tests.
Imaging tests
Doctors may use the following imaging tests to reveal areas of lung tissue with cancer:
- X-ray
- CT scan
- MRI
- PET CT
Scans can help track treatment progress and reveal changes to bones and other organs if the cancer has spread.
Tissue sampling
A healthcare professional may wish to take a biopsy using a fine needle or a bronchoscope to check for cancer cells.
For less accessible lesions, they may use a more invasive surgical procedure, such as thoracoscopy or video-assisted thoracic surgery, to remove lung tissue.
Other samples
Laboratory tests can also reveal whether or not cancer is present in the following:
- pleural effusion, which is the fluid that collects around the lungs
- sputum
- blood
This information can help confirm whether cancer is present and, if it is, determine its type and stage.
Cervical Cancer: Preventable Yet Prevalent
Cervical cancer ranks as the second most common cancer among Indian women, following breast cancer. In 2023 alone, India saw an estimated 127,526 new cases, with numbers continuing to rise. The country also records the highest incidence of cervical cancer in Asia.
Fortunately, cervical cancer is largely preventable through HPV vaccination, routine screening (Pap smears and HPV tests), and early treatment of precancerous lesions. Public health experts urge women to prioritize regular screenings and vaccinations to reduce risks.
How do healthcare providers diagnose cervical cancer?
Screening Tests
- Pap test:This test collects cells from the cervix to check for abnormal changes that may indicate precancerous or cancerous cells.
- HPV DNA test:This test detects the presence of specific HPV strains that are known to increase the risk of cervical cancer.
Diagnostic Procedures:
Colposcopy: A magnifying glass is used to examine the cervix and identify any abnormal areas.
Biopsy: A tissue sample is taken from the cervix for examination under a microscope to confirm the presence of cancer.
Endocervical curettage: A tool is used to collect cells or tissue from the cervical canal.
Cone biopsy: A cone-shaped piece of tissue is removed from the cervix and cervical canal.
Imaging: MRI, PET-CT, and other imaging techniques may be used to determine if the cancer has spread to other parts of the body.
Cancer Control Framework
Given the current state of rising cancer disease burden and sub-optimal quality of outcomes, there is a significant need to understand the current challenges and tailor make interventions across the different stages of disease management with a deep focus on:
1. Awareness and prevention – Modifying exposure to risk factors that potentially lead to cancer
2. Detection and diagnosis – Ensuring early detection and accurate staging of the disease
3. Treatment including palliative care – Driving multidisciplinary approach to treatment with focus on affordability, equitable access, quality of outcomes and palliative care
A comprehensive cancer control framework aims to reduce cancer incidence, morbidity, and mortality, while improving the quality of life for cancer patients. It involves a multi-faceted approach, encompassing prevention, early detection, diagnosis, treatment, palliative care, and ongoing research. This framework should address all levels of the health system to reach the entire population, including those at high risk and those diagnosed with cancer.
Key components of a cancer control framework include:
- Prevention and Early Detection:This involves reducing exposure to known risk factors, such as tobacco use and excessive sun exposure, and implementing screening programs to detect cancer early, when it is often more treatable.
- Diagnosis, Treatment, and Clinical Trials:Ensuring accurate diagnosis, providing access to effective treatments, and participating in clinical trials to improve outcomes and develop new therapies are crucial.
- Supportive Care:Addressing the physical, emotional, and social needs of cancer patients throughout their journey, including palliative care for those with advanced disease, is vital for improving quality of life.
- Awareness and Education:Raising public awareness about cancer risk factors, prevention strategies, early detection methods, and the importance of seeking timely care is essential.
- Governance and Policy:Establishing clear policies, funding mechanisms, and regulatory frameworks to support cancer control efforts at all levels of the health system is necessary.
- Surveillance and Research:Monitoring cancer incidence and mortality patterns, evaluating the effectiveness of interventions, and conducting research to improve cancer prevention and treatment are crucial for continuous improvement.
- Physical Activity and Cancer Control (PACC):This framework highlights the importance of physical activity for cancer prevention and treatment, with recommendations for specific levels of activity for different cancer stages and populations.
- Genomics in Cancer Control:Incorporating genomics into cancer control efforts can help identify individuals at higher risk, personalize treatment plans, and develop new diagnostic tools. Summary In summary, the cancer incidence burden is continuing to increase in India. Among the top five cancers in females, breast cancer was found to be the highest, followed by three female genital organs cervix, ovary and corpus uteri. Among males, three sites; lung, mouth and tongue were limited with tobacco-related cancers. A preventable measure needs to be taken for reducing the future burden of cancer. The new estimates are helpful for cancer prevention and control activities through the intervention of early detection, risk reduction and management in India. Appropriate research is, however, needed to delve deeper into the reasons of cancer burden and provide affordable solutions.