Menu
Childhood asthma is a long-term condition that affects millions of children around the world, causing breathing difficulties and potentially impacting their daily activities. As a parent, it can be distressing to witness your child struggle with such a significant health issue. However, gaining a comprehensive understanding of childhood asthma and being well-versed in effective management strategies can profoundly enhance your child’s well-being.
By staying informed about childhood asthma—understanding its triggers, recognizing symptoms, and grasping its impact on your child’s physical and mental health—you can provide robust support for their overall well-being. Developing an understanding about the diagnostic tests and effective management strategies equips you with essential knowledge in critical times. This approach ensures you can manage your child’s asthma effectively, allowing them to lead a happy, healthy life.
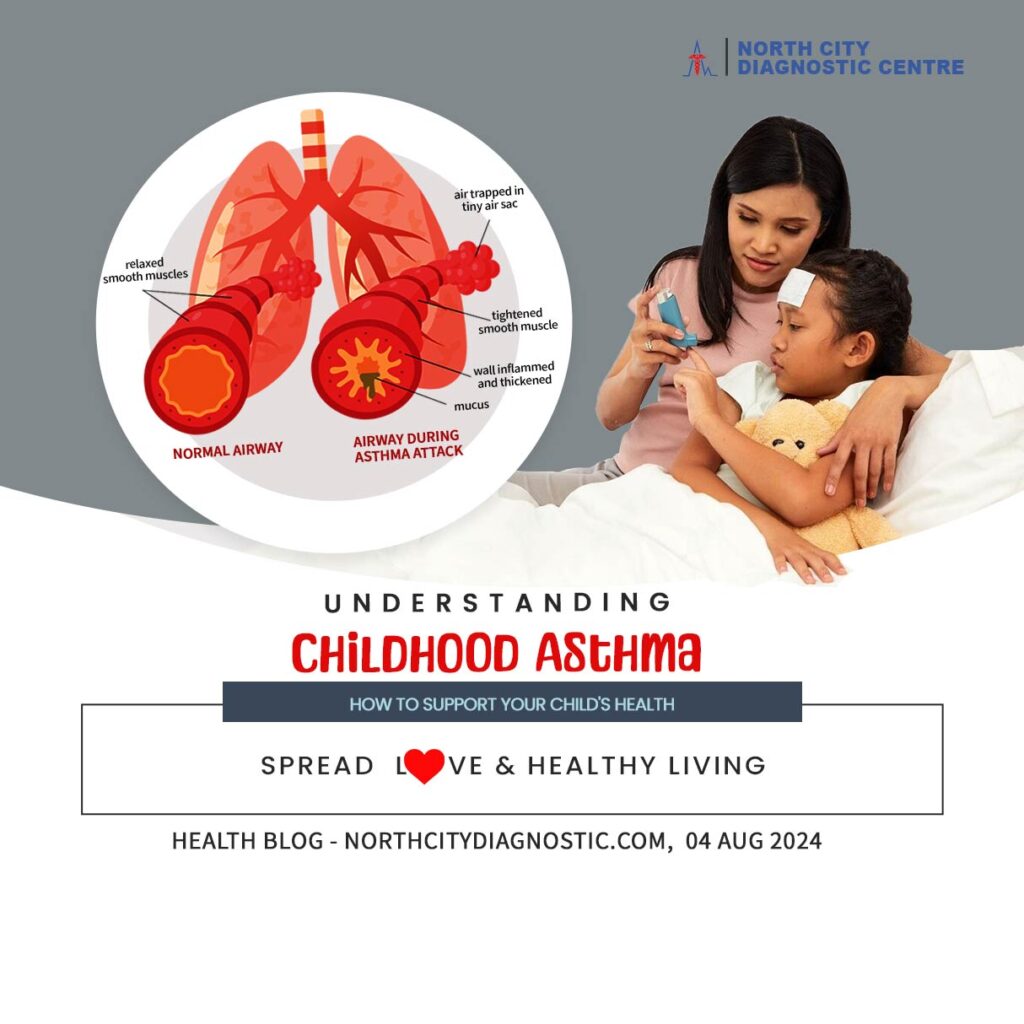
Asthma is a chronic lung disease that affects the airways, which are the tubes that carry air in and out of the lungs. People with asthma experience difficulty in getting air into their lungs because the airways become inflamed and narrow. This can lead to symptoms such as wheezing, coughing, and chest tightness. Certain triggers can exacerbate these symptoms, leading to an asthma attack. These attacks can occur suddenly or develop gradually, and in severe cases, they can be life-threatening.
Asthma can start at any age, but it often begins in childhood when the immune system is still developing. Most children experience their first asthma symptom by the age of 5. Asthma can disrupt a child’s schooling and may even require hospitalization. It’s crucial to have a treatment plan in place to effectively manage a child’s asthma.
During an asthma attack (asthma exacerbation), symptoms may intensify significantly and can be life-threatening. Seek immediate medical help if you observe:
The exact cause of asthma is not known, but it commonly develops in childhood as the immune system matures. Contributing factors include:
Asthma is not contagious. It is not caused by germs and cannot spread from person to person.
Several factors increase the risk of developing asthma:
By following these strategies, managing your child’s asthma will become a routine part of daily life, improving their overall well-being and minimizing disruptions.
At North City Diagnostic Center we offer personalized testing schedule that aligns with your medical history and risk factors. Consistent monitoring can be invaluable for early detection and effective management of arthritis. It’s not just about how often you test but making sure that the tests are aligned with your overall health profile for maximum benefit.
#ChildhoodAsthma #AsthmaManagement #SupportChildHealth #AsthmaCare #PediatricAsthma #AsthmaTips #AsthmaTreatment #ChildHealth #AsthmaSupport #AsthmaStrategies #PathologicalTest #HealthFirst #NDC #NorthCity #DiagnosticServices
35-A ,Canal West Road
Near Gouri Bari Bus Stop
Kolkata – 700004.
Local: +91 33 6605 0888