Menu
Few creatures wield as much power in the intricacy of human life on Earth as the small but deadly mosquito. These buzzing insects, which we consider as minor nuisances, can be a formidable foe who deserves our attention more than we realize. Aside from irritating bites and nightly serenades, the vector borne diseases caused by mosquitoes have a devastating effect on humanity, causing more deaths than terrorism and wars put together.
Today in through this article we will take an overview on commonly occurring vector borne-diseases caused by mosquitoes, the risks associated, preventions and other insights. After all its World Mosquito Day today!
Mosquito Facts

“If you think you are too small to make a difference, you haven’t spent the night with a mosquito.”
– African proverb quoted by the Dalai Lama.
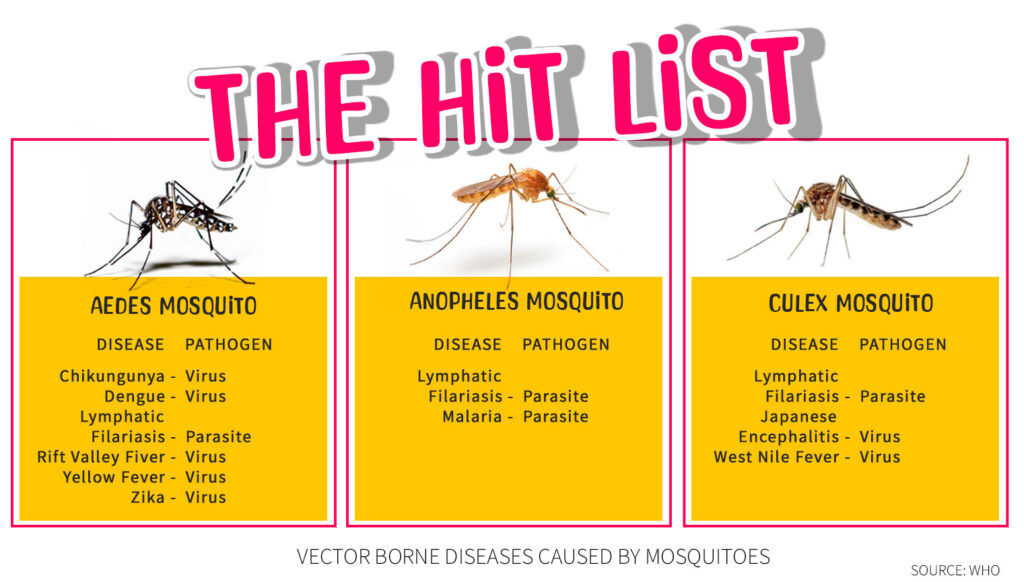
Mosquitoes are infamous for transmitting a range of diseases, significantly impacting both humans and animals. Let’s explore some of the most prevalent vector-borne diseases associated with these pesky insects. Below we will discuss about Dengue, Malaria, and Lymphatic Filariasis.
Avail specialized health check-up and screening. North City Diagnostic Centre offers state-of-the-art health check-up and screening packages at affordable prices. Call 
Home Collection available for Blood Tests related to Vector-Borne Diseases
Malaria, a life-threatening disease, is primarily transmitted through the bite of infected female Anopheles mosquitoes. The parasite responsible for malaria, Plasmodium, infects both humans and mosquitoes, perpetuating a vicious cycle of transmission.
Female mosquitoes require blood to nourish their eggs, and during this feeding process, they can transmit diseases like malaria. The Anopheles mosquito species, particularly Anopheles gambiae and Anopheles funestus, are known vectors for malaria transmission.
For this test, a drop of your blood is put on a special slide. A laboratory professional will examine the slide under a microscope to look for parasites. This test can identify all types of malaria parasites.
This test looks for certain proteins that come from malaria parasites. It can provide results in under 15 minutes, but an RDT can’t accurately show which type of malaria parasite you have. This information affects your treatment. So, if an RDT shows that you have malaria, a blood smear is needed, too.
In October 2021, the WHO approved the RTS,S/AS01 (RTS,S) malaria vaccine for administration in four scheduled doses in children five months of age to reduce the burden and severity of malaria.
Dengue fever, transmitted by the Aedes mosquito, has been on the rise globally. It causes high fever, severe joint and muscle pain, and in severe cases, it can lead to dengue hemorrhagic fever, which can be fatal.
The Aedes mosquito, namely Aedes aegypti, is the principal vector responsible for dengue virus transmission. As they deposit their eggs in clean-standing waters such as flower pots, abandoned tyres, and water storage containers, this mosquito species is well suited to urban environments. Another vector that can spread the virus is Aedes albopictus, also known as the Asian tiger mosquito.
Most dengue patients have little or no symptoms and recover in 1-2 weeks. Dengue fever can be fatal in rare cases.
Symptoms often appear 4-10 days after infection and persist 2-7 days. Symptoms could include:
Severe Dengue symptoms often show up after the fever has subsided:
This test is generally done during the first 5 days of the beginning of symptoms. This is because NS1 antigen appears on the first day of dengue infection and can last for only up to 5-7 days.
This test is also used to detect dengue virus in the early stages of the disease (first 5 to 7 days). It identifies the viral genome (the virus’s genetic material) in the blood. This test is approximately 90% sensitive and 95% specific in detecting the infection.
This test detects IgM (antibodies) in the blood, which appear in the initial phase of the disease, and signifies acute infection or recent infection. It is usually done after the 4th day of the occurrence of the symptoms as the antibodies start developing after 4-5 days of infection.
The test is used to detect infection in the later course of the disease because the level of IgG which is to be monitored in the test tends to increase slowly. You can get an IgG antibody test for dengue after 14-21 days of infection or even later as these antibodies remain in the blood several months post infection.
Dengue is frequently associated with decreased platelet count (normal platelet count lies in the range of 1.5 to 4 lacs). Therefore, platelet count should be monitored carefully and regularly, especially when the fever comes down.
The dengue vaccine CYD-TDV or Dengvaxia was approved by the US Food & Drug Administration in 2019, the first dengue vaccine to get the regulatory nod in the US.
Researchers at India’s National Centre for Biological Sciences, in collaboration with nine other institutions in India, Africa, and the US, have developed India’s first and only DNA vaccine candidate for dengue fever.
Lymphatic filariasis, often known as elephantiasis, is a parasitic illness caused by filarial parasites, which are thread-like worms. Elephantiasis infects 120 million people a year in Africa and Asia.
The bites of infected mosquitos, notably those of the Anopheles, Culex, and Aedes genera, spread this illness to people. The infection predominantly affects the lymphatic system, which is responsible for fluid balance and immunological responses in the body.
Mosquitoes are infected with microfilariae by ingesting blood when biting an infected host. Microfilariae mature into infective larvae within the mosquito. When infected mosquitoes bite people, mature parasite larvae are deposited on the skin, from where they can enter the body. The larvae then migrate to the lymphatic vessels where they develop into adult worms, thus continuing a cycle of transmission.
Lymphatic filariasis infection involves asymptomatic, acute and chronic conditions.
A physical check-up by your doctor can determine if you have elephantiasis. They will inquire about your medical history and if you have travelled to a location where elephantiasis is more prone to occur.
Blood tests will be performed to determine whether roundworms are present in your circulation. These tests must be performed at night since that is when these parasites are most active.
A paramount tactic in thwarting the proliferation of vector-borne maladies encompasses the obliteration of mosquito breeding locales. Any residual waters, be it in plant containers, discarded tires, or eaves, possess the potential to function as founts of propagation.
Employing insect repellents housing DEET, picaridin, or other endorsed substances offers a defensive barrier against mosquito stings. Donning attire with elongated sleeves and trousers similarly mitigates vulnerability to mosquito nibbles.
Resting beneath bed nets imbued with insecticidal properties manifests a substantial reduction in the hazard of nocturnal gnawing. Affixing screens to apertures and entrances serves to hinder the ingress of mosquitoes into habitation precincts.
It is preferable to get tested in case the symptoms shows. Always consult a doctor.
Home Collection available for Blood Tests related to Vector-Borne Diseases
Call 
Integrated Pest Management (IPM) involve an all-encompassing approach to regulating overall mosquito population. This entails the utilization of pesticides, biologically based control methods, and community based activities to minimize the spread of diseases.
The scientific community is actively probing the feasibility of genetically modified mosquitoes, bereft of the capability to transmitting diseases. This innovative approach holds the potential to reduce disease transmission without harming the ecosystem.
While we love the summer warmth and the rainy reliefs, it is critical to be mindful of the underlying dangers presented by mosquitoes. Individuals and communities can be devastated by vector-borne diseases. We can reduce the burden of these diseases and create a safer environment for everybody by adopting preventative actions and supporting new methods.
#MosquitoMysteries #BiteBackBattles #BuzzKillers #SkeeterSecrets #MosquitoMenace #BuggingOut #DiseaseDodge #VectorVoyage #MozzieMatters #BeatTheBite #BugOff #MosquitoFacts #SquadronOfSkeeters #ItchyTruths #MosquitoPrevention #InsectIntel #BeyondBugSpray #BuzzingBeGone #ExploreAndDefend #NotTodayMosquito #NDC #NorthCityDiagnosticCentre #Malaria #Dengue #elephantiasis #VectorBorneDiseases
35-A ,Canal West Road
Near Gouri Bari Bus Stop
Kolkata – 700004.
Local: +91 33 6605 0888